Is Covid Testing Covered By Medicaid
The vast majority of schools that render school-based services covered by Medicaid are reimbursed via a. The Medicaid program pays for Coronavirus disease 2019 COVID-19 molecular antigen and antibody testing for diagnostic and screening services services ordered by a qualified provider.
Enabling pharmacies to be reimbursed for COVID testing is just one of several initiatives Ohio Medicaid has implemented since the start of the pandemic.

Is covid testing covered by medicaid. Under the Families First Coronavirus Response Act Medicare Medicaid and private health insurance plans are required to fully cover the cost of COVID-19 testing. For information on the testing and treatment of the uninsured for COVID-19 see the resources section of this page. The cost of a COVID-19 test should be fully covered by health insurance and a person doesnt have to have symptoms or exposure to someone.
Medicaid Coverage of Coronavirus Testing Alert Rapid Lab Test and Antibody Test Provider Alert Additional Guidance on Antibody Testing Alert Exceed Service LimitsExpand Coverage. The option to cover COVID-19 testing for the uninsured builds on this history. Lets say you go for your annual physical and your doctor recommends that you get a hearing and balance test.
For dually eligible individuals Medicaid may cover additional testing beyond what is covered by Medicare based on Medicaid policy. NYS Medicaid FFS will not cover tests that are over-the counter or purchased for at home use. COVID specimen collection should not be billed to Medicaid when a home health visit is covered by Medicare either episodic or Low Utilization Payment Adjustment LUPAfee-for-service payment.
Medicaid has a long history as a public health first responder. Uninsured individuals who do not qualify for Medicaid may still have to pay out-of-pocket for diagnostic testing. The American Rescue Plan Act of 2021 ARPA PL.
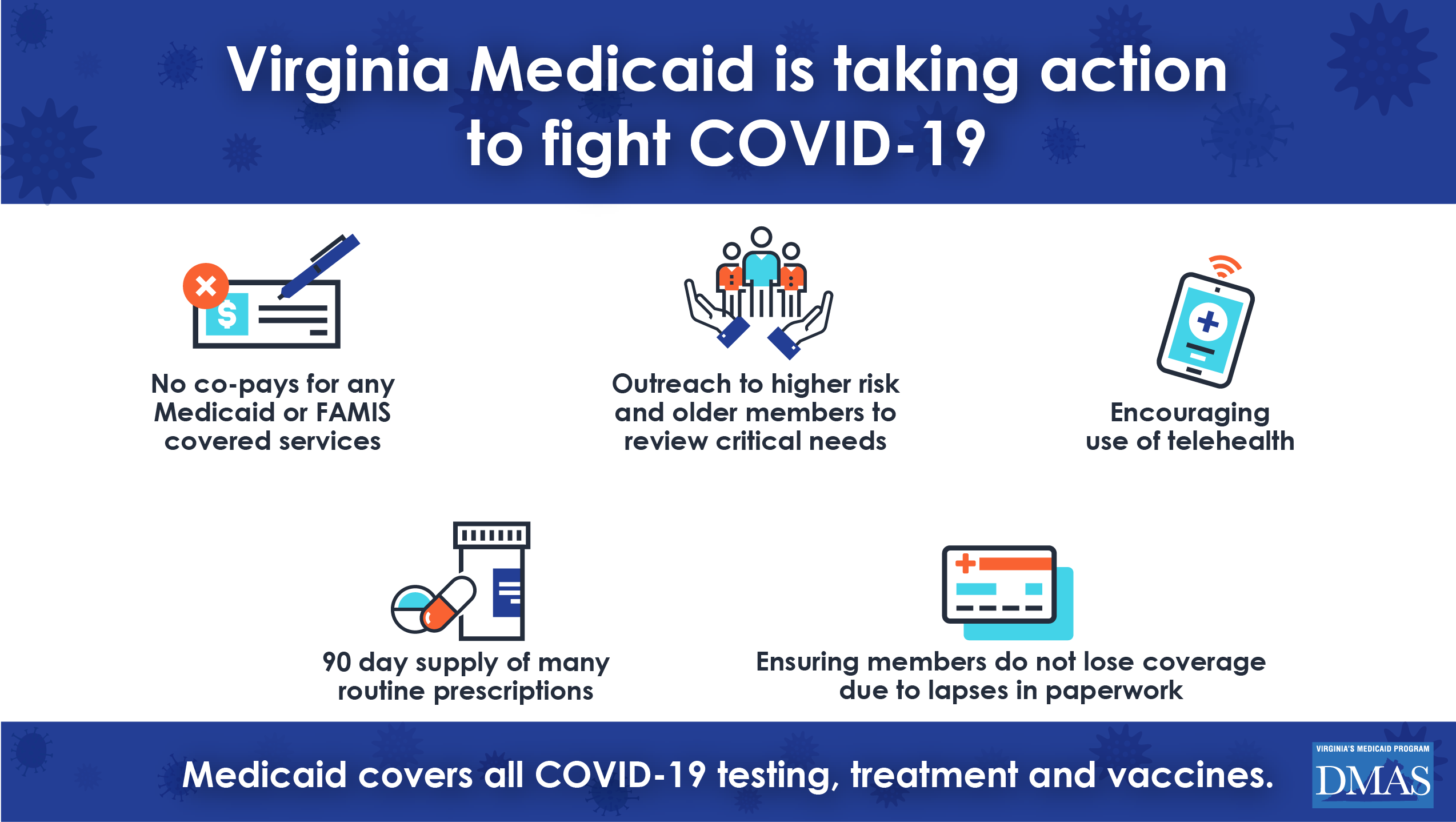
It is tied to a public health emergency declaration connected to a specific diagnosis and fully funded by. COVID-19 testing is a covered benefit for current Healthy Connections Medicaid members including those enrolled in Family Planning so they do not need to apply for the new program. During the Public Health Emergency PHE and for more than a year after it ends Medicaid is required to cover COVID-19 testing vaccinations and treatment for most enrollees and it may not charge cost sharing for these services.
Coverage of COVID-19 vaccine administration is mandatory for most Medicaid beneficiaries both adults and children without cost-sharing during the period when section 1905a4E added by the ARP and the corresponding amendments to sections 1902a10 1916 and 1916A of. But plans that arent considered minimum essential coverage arent required to cover COVID-19 testing. Schools can be Medicaid providers of COVID-19 screening testing covered under section 1905a4F and the other amendments made by section 9811 of the ARP.
The law does not specify who can provide diagnostic testing nor does it include a reimbursement amount. Exceed service limits to maintain the health and safety of recipients diagnosed with COVID-19 or when it is necessary to maintain a recipient safely in their home. When tests are available for you in your state Medicare covers and you pay nothing for.
No prior authorization will be required on the COVID-19 lab test by Medicaid and CHIP health plans or by traditional Medicaid. Medicaid and CHIP will cover COVID-19 testing for Medicaid or CHIP clients. As of June 29 2020 Ohio pharmacies serving Medicaid beneficiaries can submit COVID-19 diagnostic testing claims for reimbursement by the Ohio Department of Medicaid ODM.
Medicaid and CHIP will cover COVID-19 testing for Medicaid and CHIP clients. For State Medicaid and Childrens Health Insurance Program CHIP Agencies. Qualified providers are those who are eligible to bill Medicaid for reimbursement such as health care providers pharmacists and dentists as listed in.
Coverage and Benefits Related to COVID-19 Medicaid and CHIP Medicaid and the Childrens Health Insurance Program CHIP provide health coverage to millions of Americans including eligible low-income adults children pregnant women elderly adults and people with disabilities. ARPA also required Medicaid limited COVID-19 testing plans to cover COVID-19 treatment. No prior authorization will be required on the COVID-19 lab test by Medicaid and CHIP health plans or by traditional Medicaid.
Your healthcare provider will work with local public health officials to determine if you should be tested for COVID-19. Or an electrocardiogram EKG. Tests to diagnose or aid the diagnosis of COVID-19.
Medicare is the primary payer for most Medicare covered testing for beneficiaries enrolled in Medicare including Medicare -Medicaid dually eligible individuals. The Centers for Medicare Medicaid Services CMS released six sets of general Frequently Asked Questions FAQs to aid state Medicaid and Childrens Health Insurance Program CHIP agencies in their response to the coronavirus disease 2019 COVID-19 pandemic. SCDHHS has also made a number of temporary policy changes to ensure ongoing access to care during the COVID-19 pandemic including creating additional ways to submit documents electronically to the.
On June 12 2020 the Agency provided guidance on Florida Medicaid coverage requirements for the antibody test. NYS Medicaid FFS will cover COVID-19 specimen collection or CLIA waived COVID-19 testing at pharmacies in accordance with the PREP Act. The Families First Coronavirus Response Act HR6201 signed into law on March 17 requires nearly all health plans including Medicare and Medicaid to pay for COVID-19 testing including the lab fees and the fees associated with the doctors office urgent care clinic or emergency room where the test is administered.
Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test. Preliminary Medicaid CHIP Data Snapshot Services through May 31 2020 PDF 112 MB. Or a Hepatitis B screening.
Medicaid covers COVID-19 laboratory testing. It is groundbreaking for several reasons. Services Delivered via Telehealth Among Medicaid CHIP Beneficiaries During COVID-19.
Medicaid and CHIP are funded jointly by states and the. The purpose of this alert is to clarify Medicaid coverage of additional procedure codes used. Preliminary Medicaid CHIP Data Snapshot Services through June 30 2020 PDF 3134 KB Service use among Medicaid CHIP beneficiaries age 18 and under during COVID-19.
117-2 included a requirement that most Medicaid limited-benefit plans cover COVID-19 vaccine administration effective March 11 2021. Thus subject to plan agreements and state scope of practice pharmacists may be able to provide COVID-19 diagnostic testing.
Key Questions About The New Medicaid Eligibility Pathway For Uninsured Coronavirus Testing Kff

Covid 19 Resources For Health Care Access In Washington State Northwest Health Law Advocates

Covid 19 Test Pricing Precios De La Prueba Covid 19
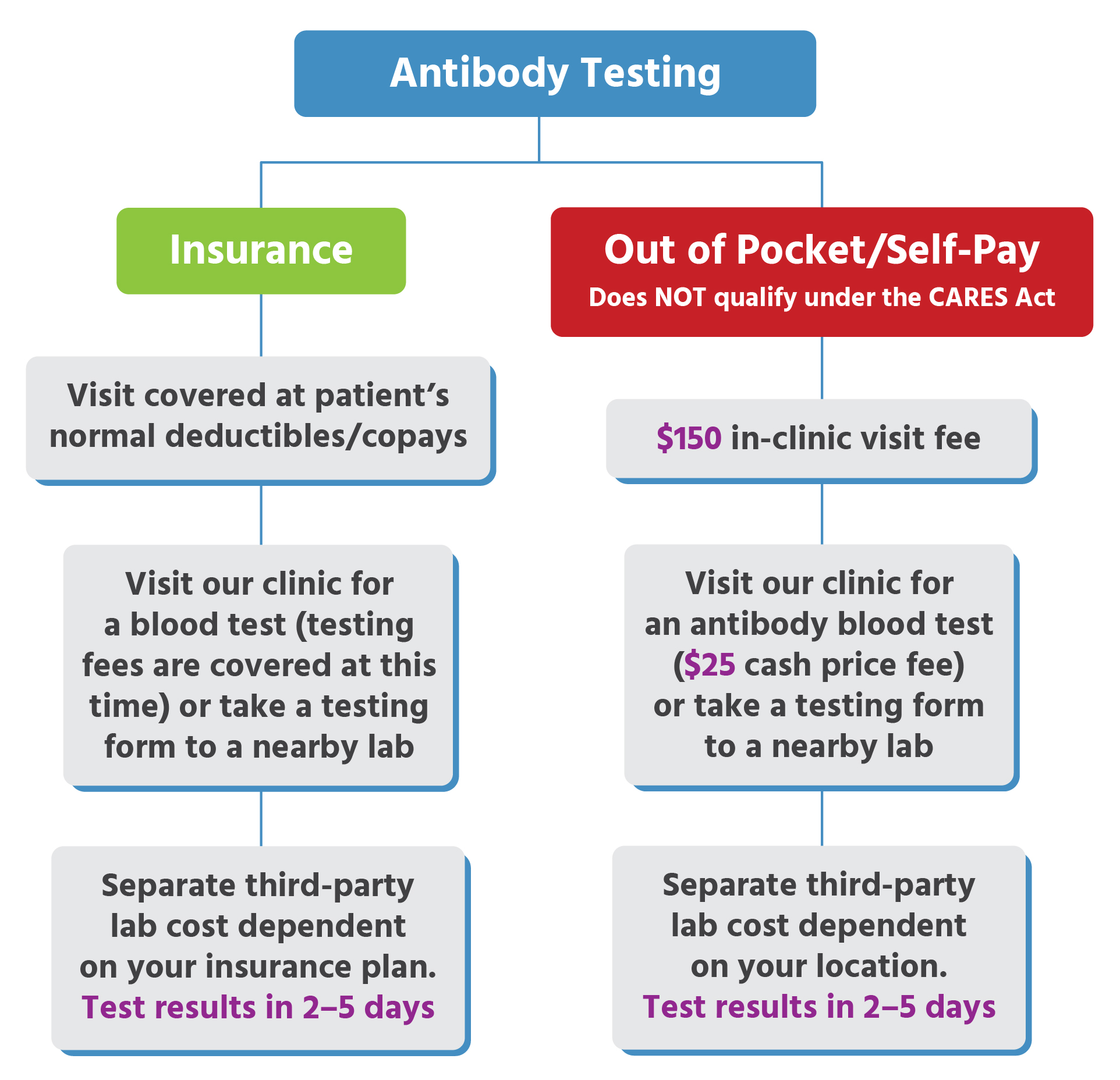
Urgent Care For Kids Antibody Testing Locations
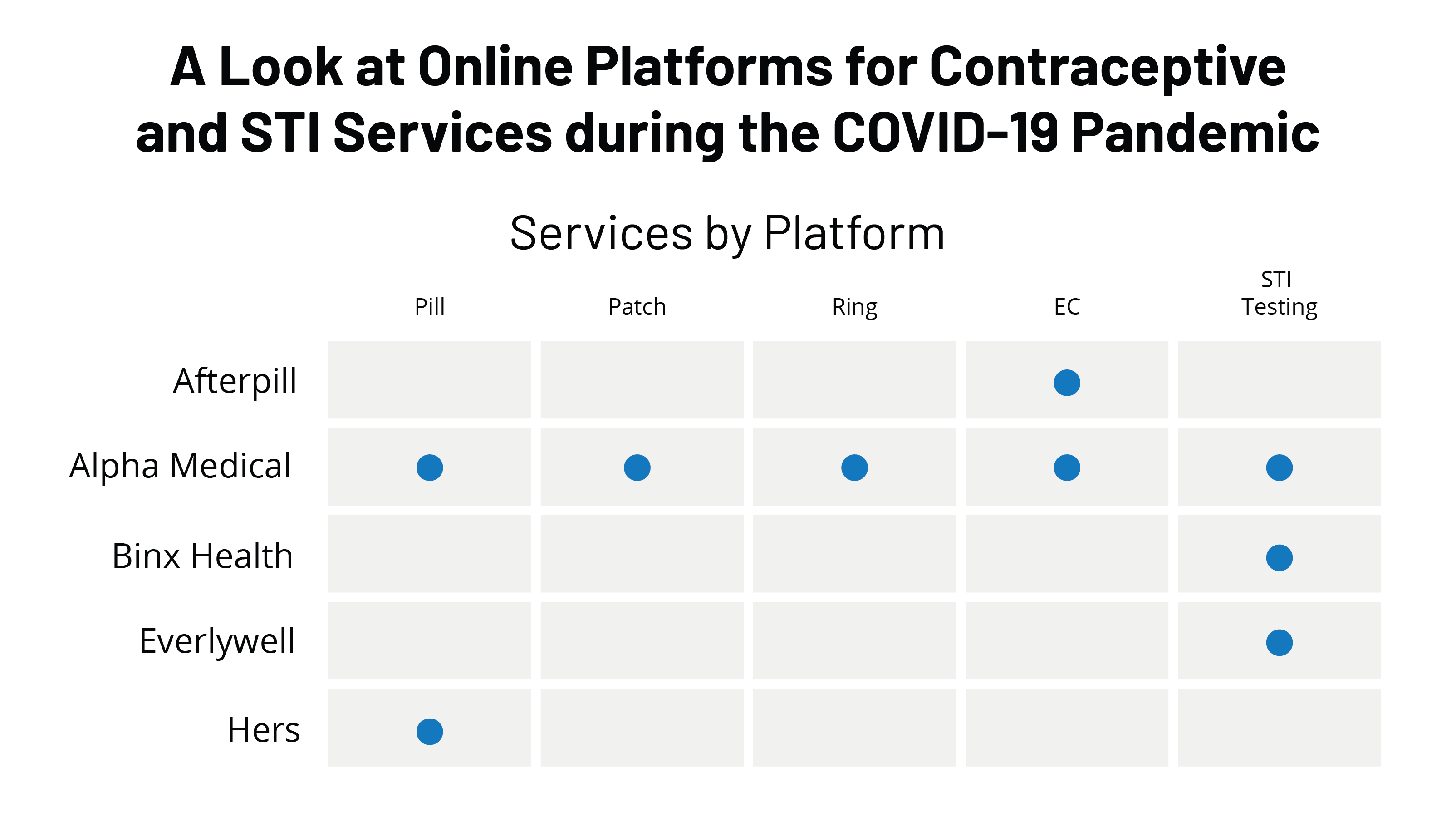
A Look At Online Platforms For Contraceptive And Sti Services During The Covid 19 Pandemic Kff
Faqs On Medicare Coverage And Costs Related To Covid 19 Testing And Treatment Kff
![]()
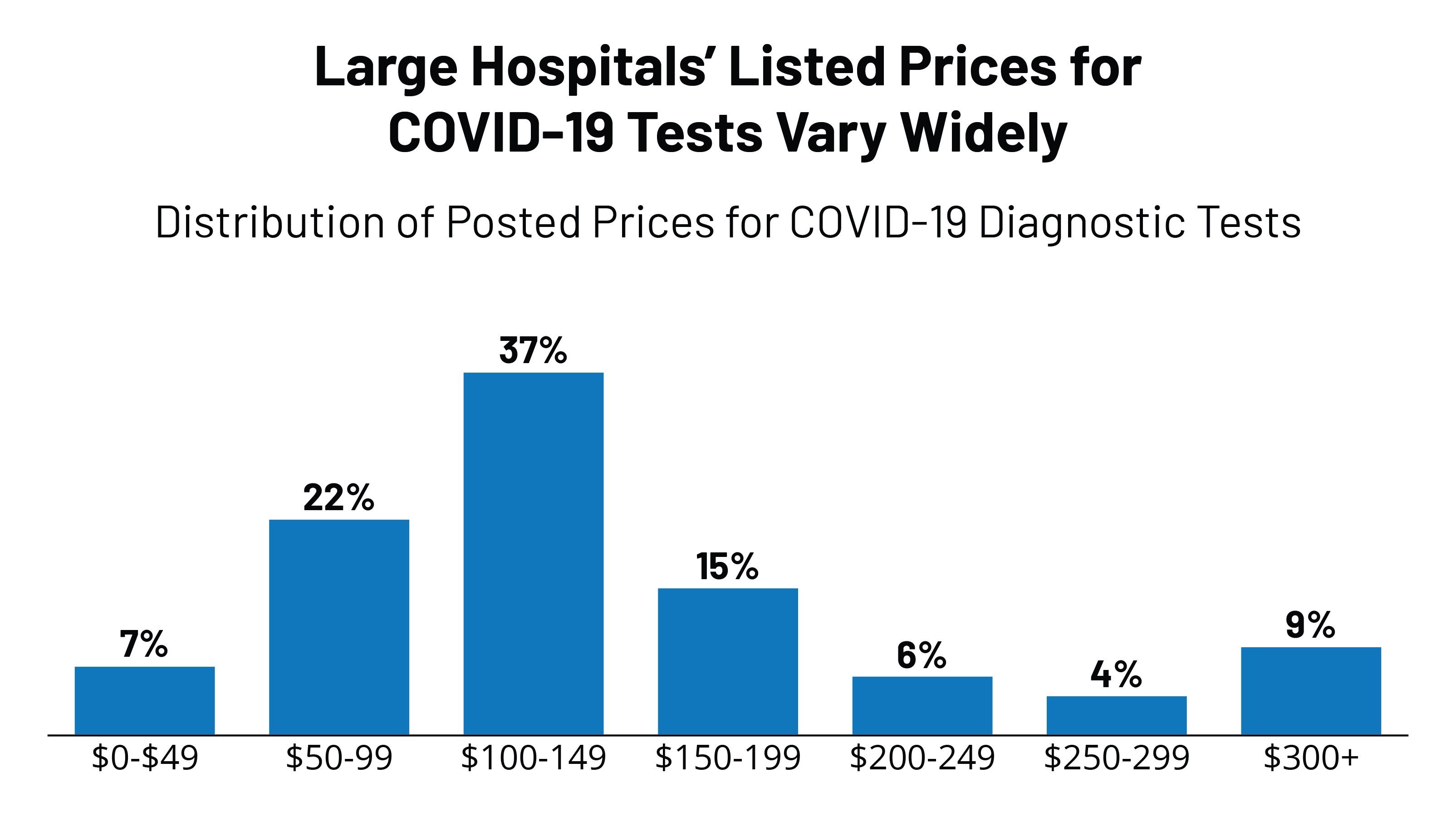
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker

Medicaid And Chip Flexibility Can Help Safeguard Americans During The Covid 19 Crisis Urban Institute

Mandatory Vaccination For Workers In Medicare Medicaid Participating Facilities Under President Biden S Plan Cda
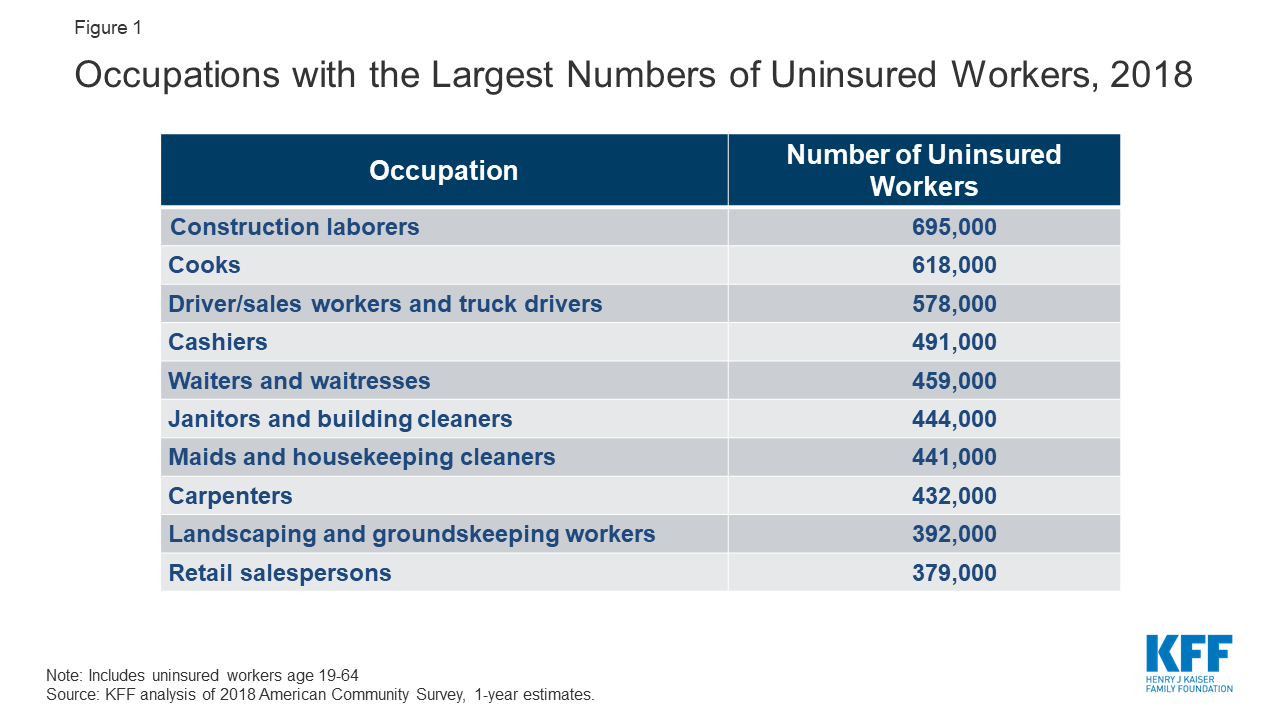
What Issues Will Uninsured People Face With Testing And Treatment For Covid 19 Kff

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff

How Long Covid Is Forcing A Reckoning With The Neglect Of Post Infectious Chronic Illnesses Bill Of Health
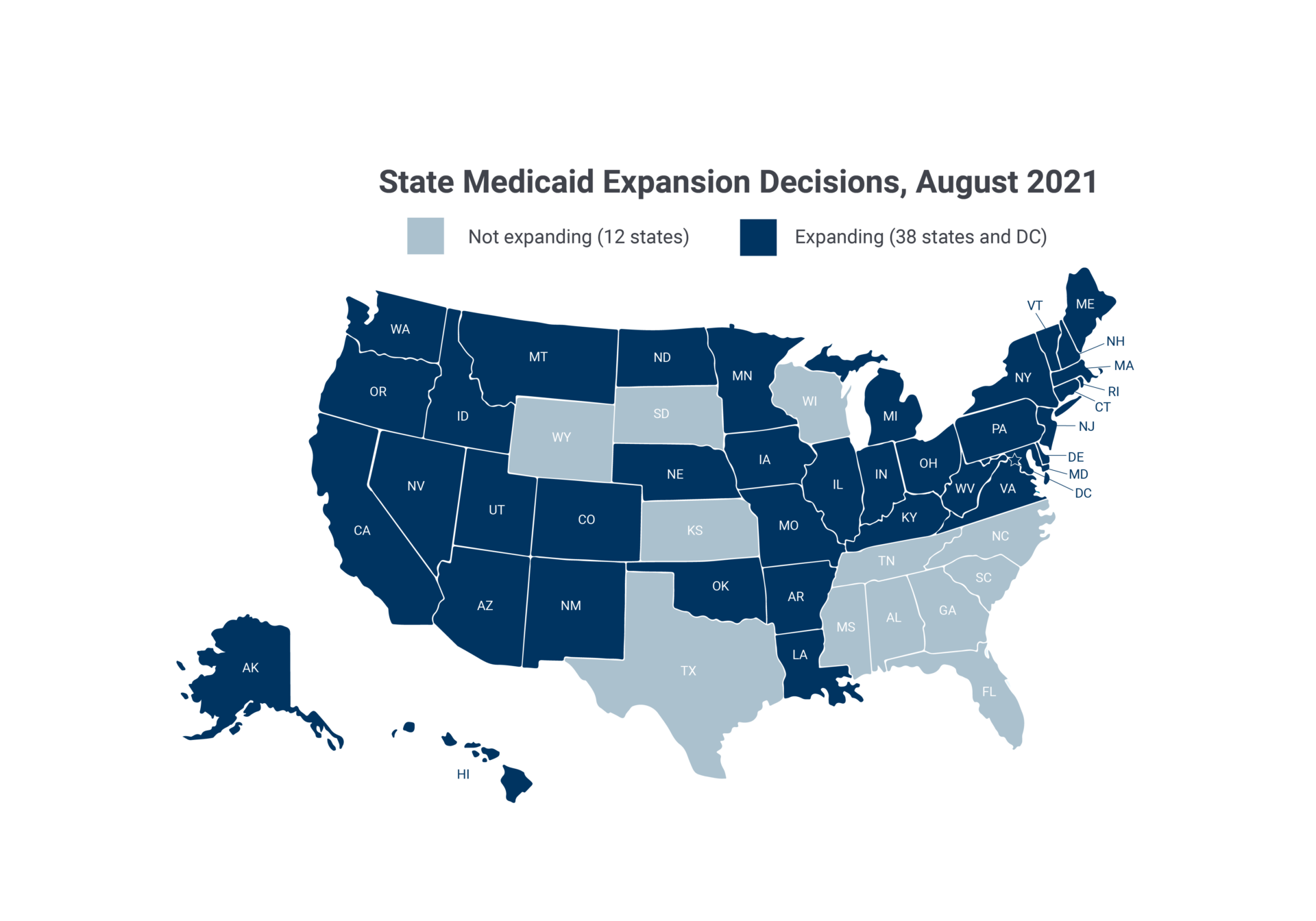
Medicaid Expansion To The New Adult Group Macpac
What S In A Covid 19 Test Northwell Health

Nuevas Pruebas De Covid 19 Sin Ir A Un Laboratorio

The Laws Governing Covid 19 Test Payment And How To Improve Them


Posting Komentar untuk "Is Covid Testing Covered By Medicaid"