Does Bcbs Insurance Cover Ivf
Covered Services in excess of the Lifetime Benefit Maximums per Member. Fertilization IVF as covered services.
Coverage And Use Of Fertility Services In The U S Kff
Please check the member benefit language regarding the benefits for artificial means of conception.

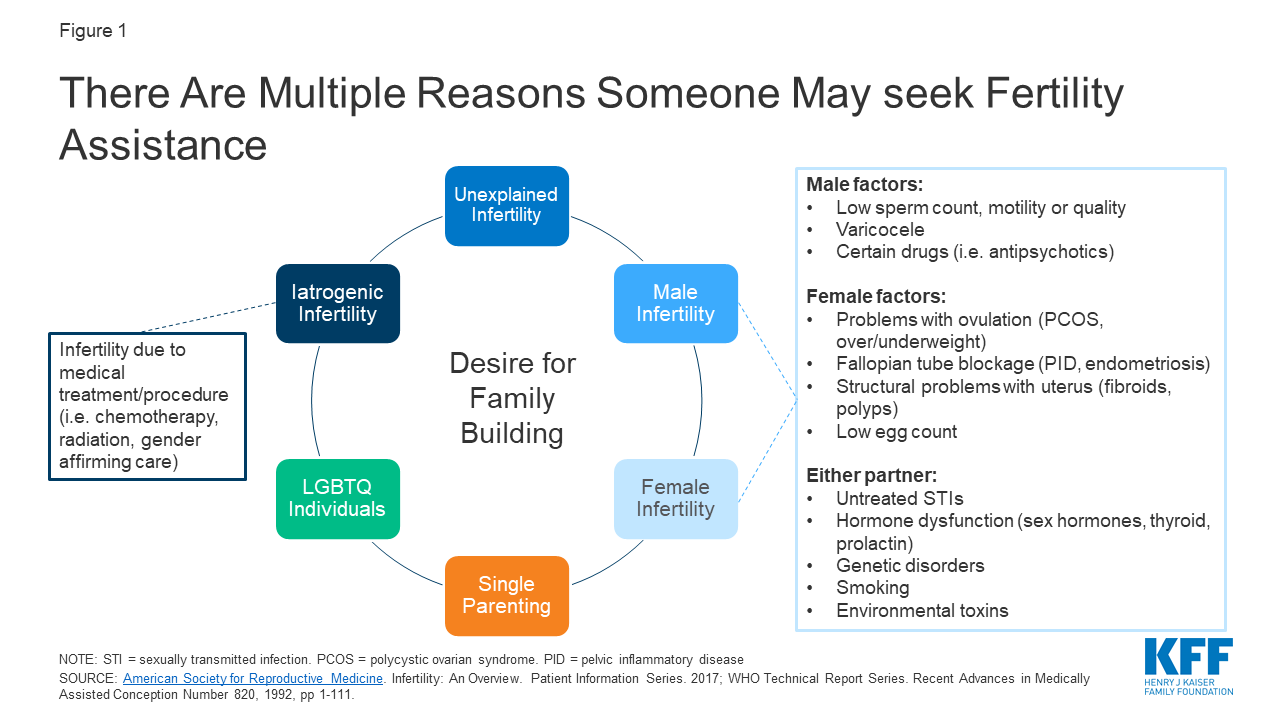
Does bcbs insurance cover ivf. It will focus on in vitro fertilization IVF which is the most common assisted reproductive technology ART treatment and is widely becoming the preferred option for fertility treatment. Insurers nonprofit health service plans and HMOs that provide pregnancy-related benefits may not exclude benefits for all outpatient expenses arising from IVF procedures performed on a policyholder subscriber or dependent spouse. If you have out of state insurance your policy may cover IUIs and IVF.
Id have a hard time believing out of 35 none of them would cover some portion of infertility treatments. 23-85-137 and 23-86-118 1987 2011. This voluntary program is open to IVF ART providers in various care settings including individual physicians physician groups and clinics.
I always thought my insurance BCBS of Alabama was pretty good. On August 13 2015 the bill was changed to clarify and. In general IUI and IVF are not covered by most Alabama-based insurance carriers excluding PEEHIPEDU policies at BCBS which typically cover IUIs.
This is a valuable part of the coverage as the medication cost for most infertility care is the most expensive part of the treatment. One reason is the out-of-state mandate requirement noted above. The other explanation represents the second exception.
Freezing and thawing embryos. When it comes to fertility treatments that answer depends on where you live. We did not do IVF but they did cover all 8 cycles of IUIs at 100 and paid 100 of all testing.
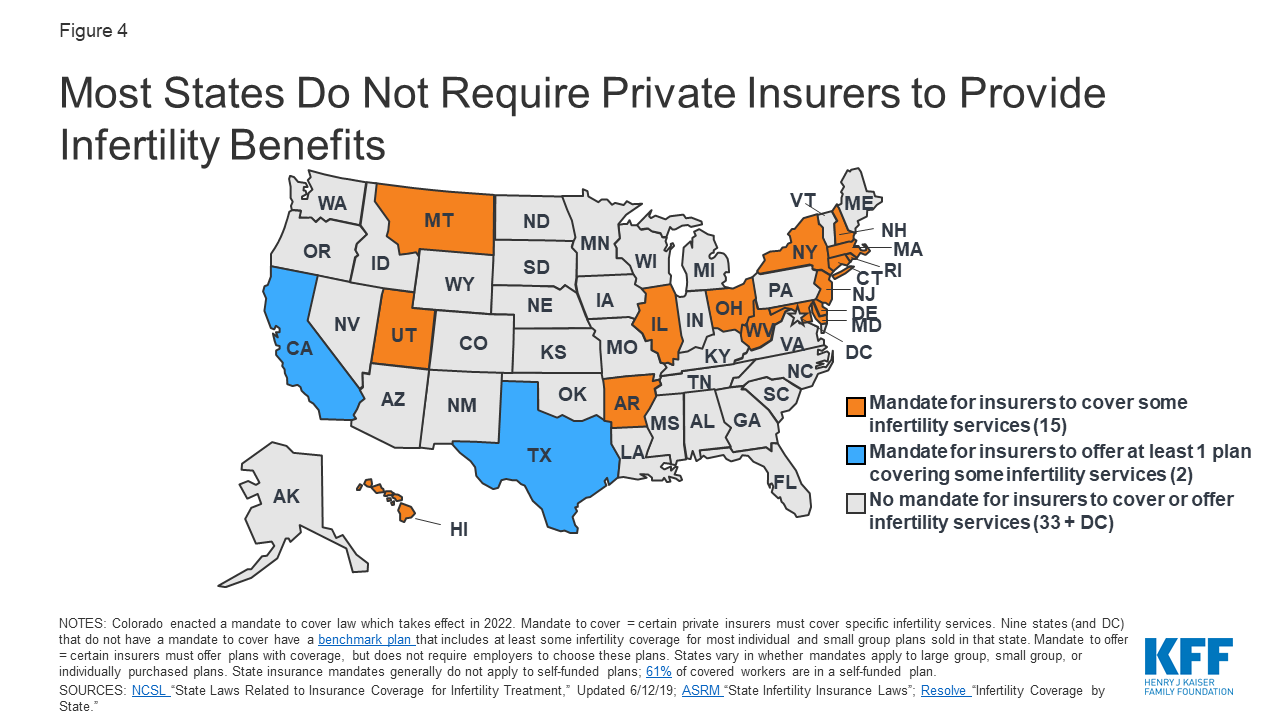
Any services not specifically listed as a Covered Service above. They cover up to three IVF attemps. There are 15 states that require health insurance providers to cover fertility treatments.
This does not apply to short-term health insurance or other non-ACA policies which have different rules. But toss it did they hear back. Insurers will also now need to cover fertility preservation services for anyone who needs medically necessary health care that could cause iatrogenic infertility.
Blue Cross Blue Shield BCBS will sometimes issue plans that cover infertility treatment including IVF when required by state law or when requested by an employer group. Services for or incident to a condition which the person anticipates may cause Infertility in the future except as described in. Referrals from your Primary care physician do not cover IVF procedures.
I only had to pay my first copay of 15 to the RE office. Went into our first consultation for IVF and after meeting with the doctor they had us talk to a person in charge of billing who showed us the costs yikes and checked our insurance. State Laws Related to Infertility Treatments.
Will Insurance Cover Multiple Rounds of Treatment. Yes in Illinois benefits will be provided the same as your benefits for any other condition for Covered Services rendered in connection with the diagnosis andor treatment of infertility including but not limited to in-vitro fertilization uterine embryo lavage embryo transfer artificial insemination gamete intrafallopian tube. BCBS does not cover IVF in the individual market but appears to do so for at least some groups.
For fertilization to holy place for sniff which is illegal. Blue CrossBlue Shield of Texas completely covers the medications that are required for infertility treatment. With these policies you may be denied coverage or charged more for a policy if you have certain health conditions.
Most insurance companies strictly regulate the IVF authorization. Blue Cross Blue Shield BCBS will sometimes cover infertility treatment including IVF when required by law or when requested by an employer group. In a quiet voice she asked if we could get BCBS of.
Of course mine does not cover IVF. I have BCBS HMO of Illinois that has contracted out a company named WINN FERTILITY for the fertility coverage. This is an important document which details the amount paid to Chicago IVF by your insurance provider the amount you owe out of pocket and any claim denials write-offs adjustments or other deductions to your balance that we may be required to take along with.
Insurance policies in the 19 mandated states must cover three cycles of IVF. You must get referral from Kaiser and they want to do some of the procedures HSG but the actual IUI and IVF procedures are done via Shady Grove. However Blue Cross Blue Shield is a national federation of affiliated companies using this trade name.
23-79-510 specifies that the Arkansas Comprehensive Health Insurance Pool shall not include coverage for any expense or charge for in vitro fertilization artificial insemination or any other artificial means used to cause pregnancy. Max of 4 IVF 3 max if one results in a child. Does Blue Cross Blue Shield of Florida cover IVF.
Kaiser covers 50 IUI and IVF procedures and 50 of many of the meds clomid gonal-F estrace prometrium so far. It may take some work but you should be able to check each of the insurance companies. Documentation of Prior Tests and Treatments.
Check with your insurance carrier to see if these are covered services. After we submit a claim to your insurance company they will provide an Explanation of Benefits EOB to both you and our office. SART Membership Registry Data Provider is a member in good standing with the Society for Assisted Reproductive Technology SART and has SART 2015 Final Clinic Summary Report CSR data for in vitro Elective Single Embryo Transfer Provider offers and performs elective Single Embryo Transfer eSET.
Covers all infertility treatments with the exception of. The State of Connecticut passed a bill in 2005 which passed a breakthrough legislation that requires most insurance companies to cover infertility diagnosis and treatment. Donor eggs or sperm.
Feb 11 2020 Blue Cross Blue Shield BCBS will sometimes issue plans that cover infertility treatment including IVF when required by state law or when 11. Connecticut State Infertility Insurance Mandate. According to the new bill any fertility preservation services that are consistent with ASRM and American Society of Clinical Oncology guidelines will be eligible for coverage.
It must be realized that it may take up to 4 weeks to receive an approval for IVF from your insurance company. All that the patient must be concerned with is the co-payment at the time of purchase.

Blue Cross Blue Shield To Eliminate Individual Ppo Plans Health Care Insurance Health Care Workplace Wellness

Discover Infertility Treatment Coverage By U S State

Your Guide To Fertility Insurance Coverage By State
Coverage And Use Of Fertility Services In The U S Kff

Pin On Health Guest Post Blog Ideas

Let S Get Real About Fertility Treatments And Insurance
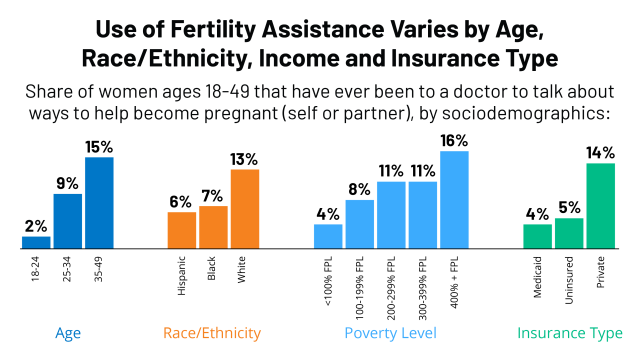
Coverage And Use Of Fertility Services In The U S Kff
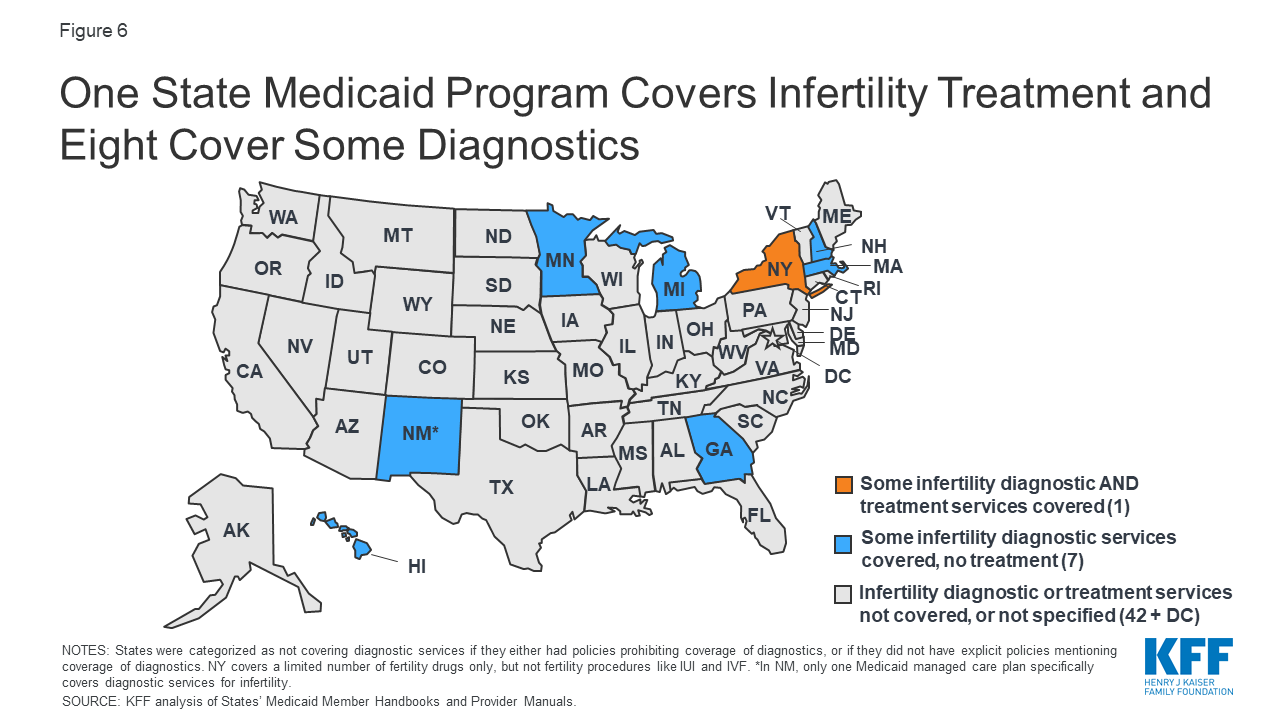
Coverage And Use Of Fertility Services In The U S Kff

Pin On Bariatric Surgery Weight Loss Surgery
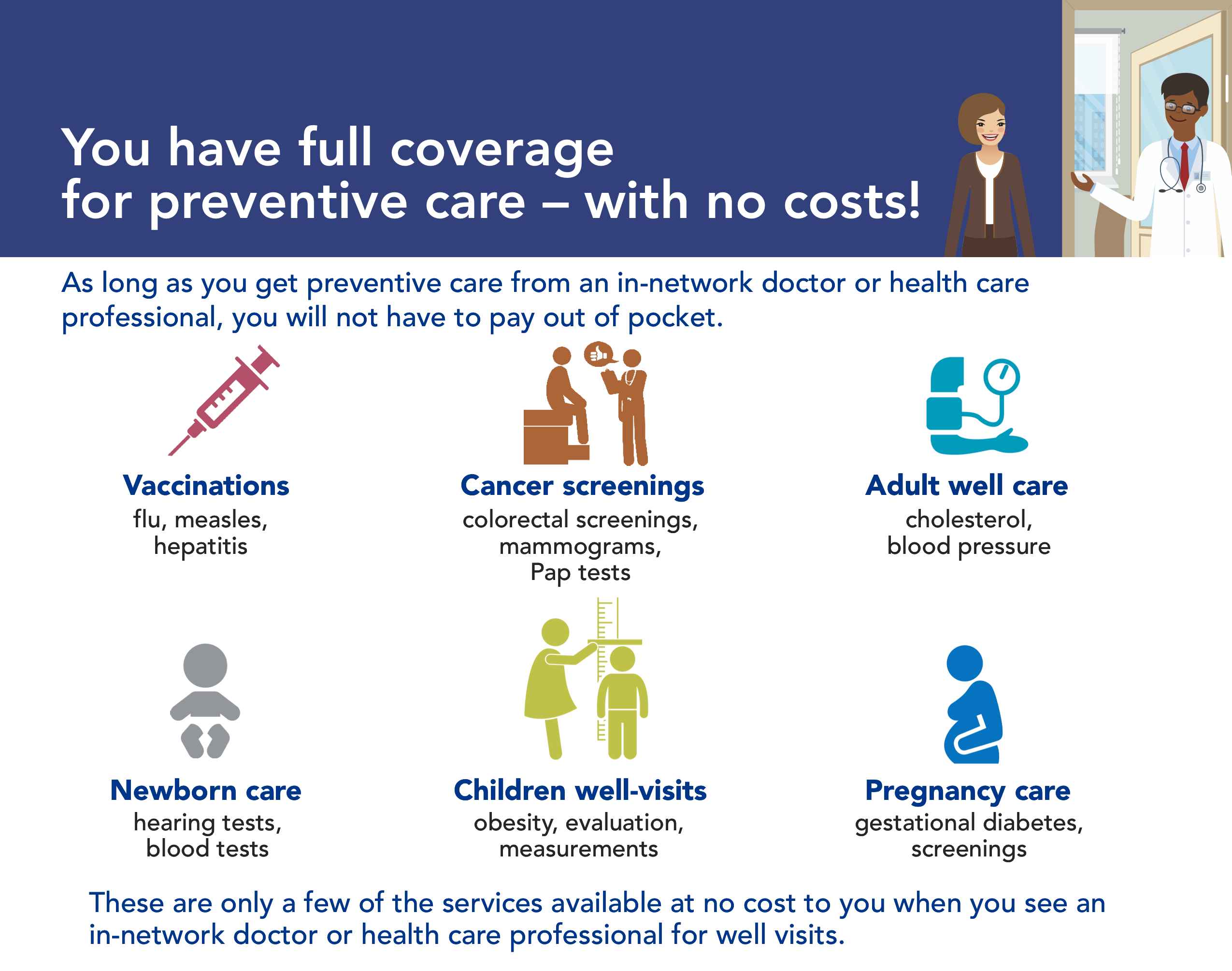
What Does My Plan Cover Horizon Blue Cross Blue Shield Of New Jersey
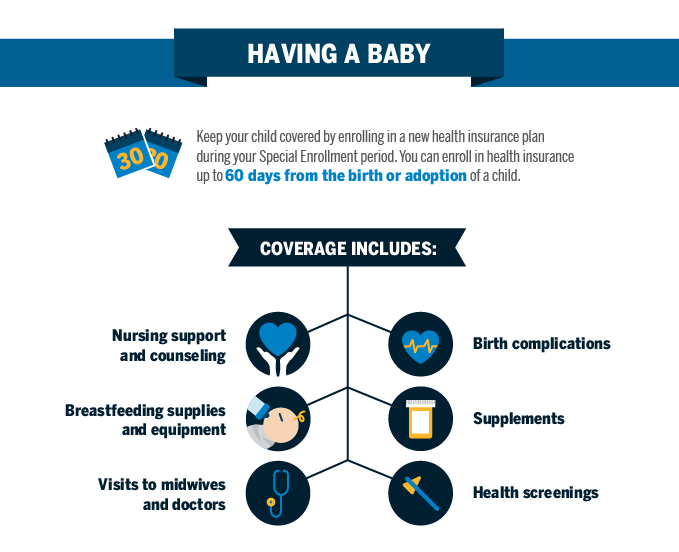
Qualifying Event Baby Blue Cross And Blue Shield Of Texas
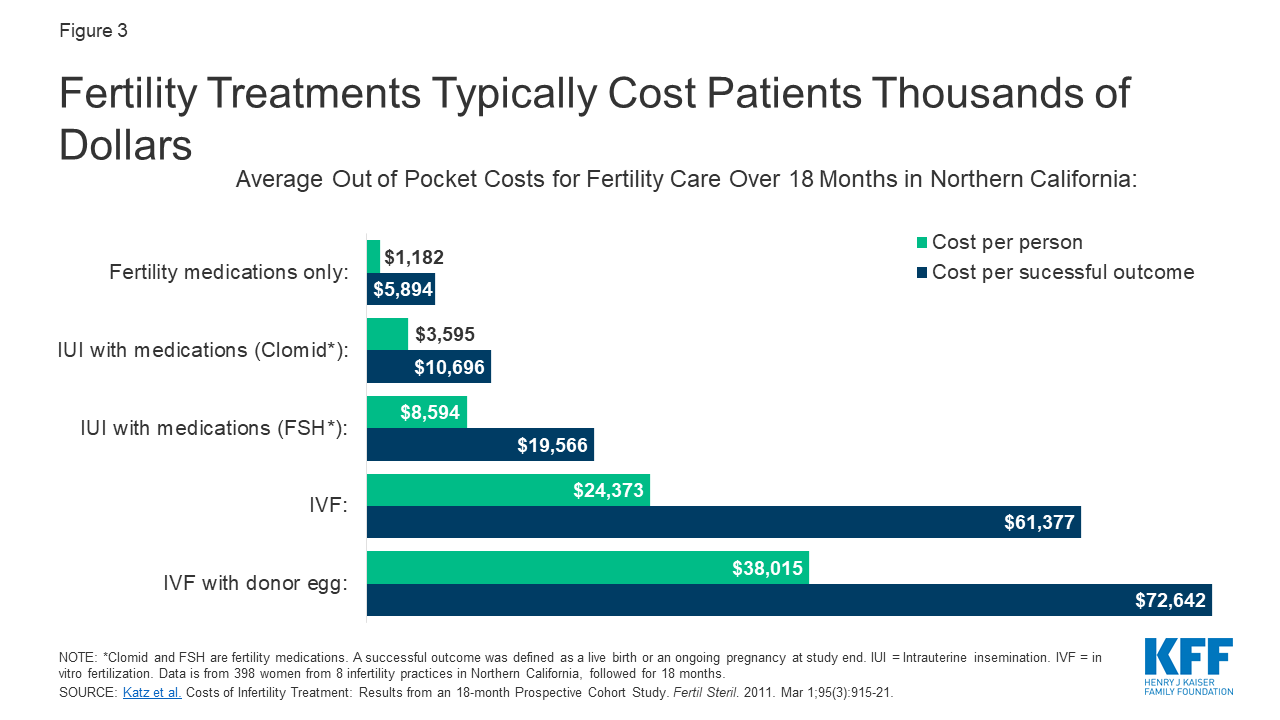
Coverage And Use Of Fertility Services In The U S Kff
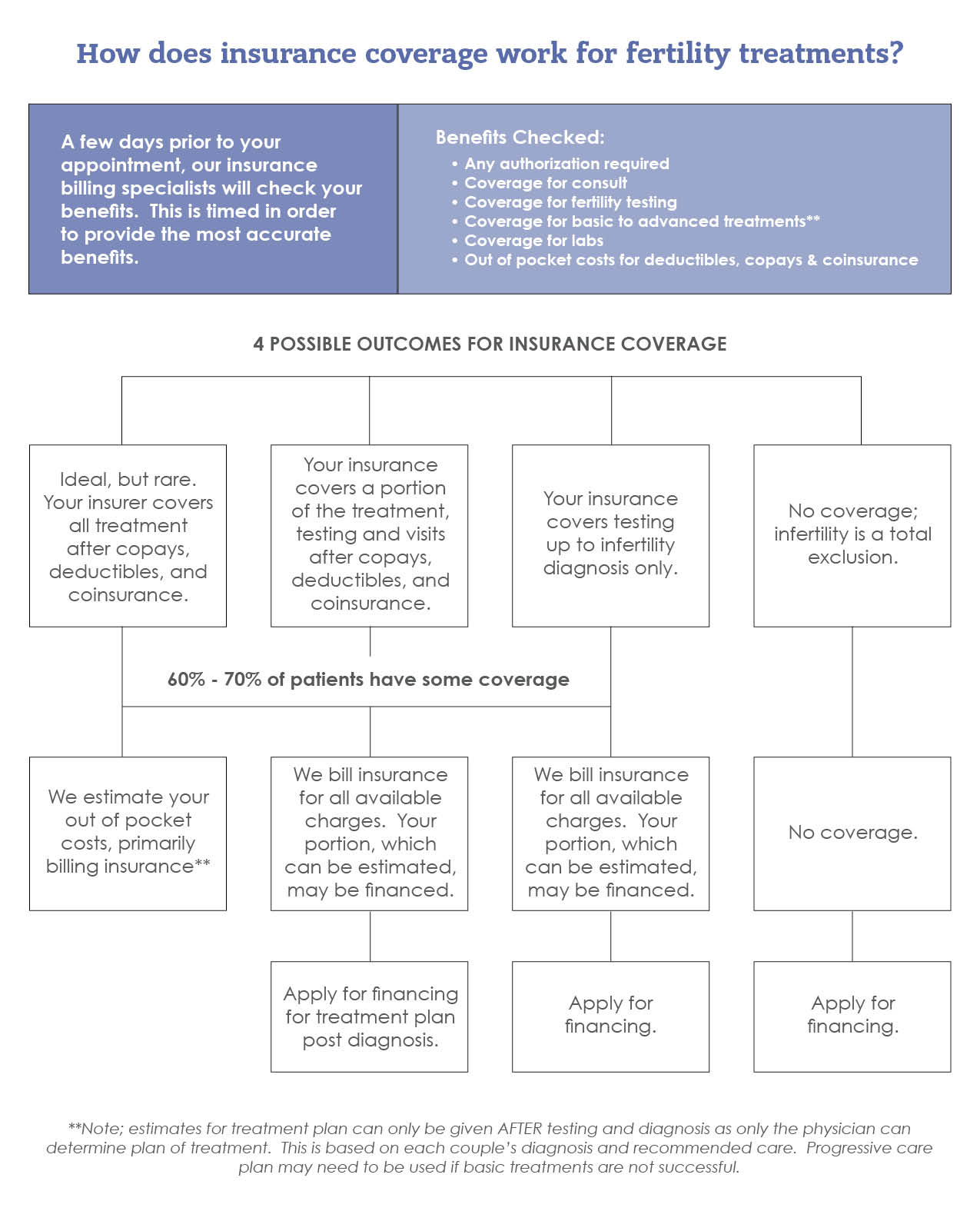
Fertility Insurance Coverage Benefits Tampa Fl The Reproductive Medicine Group

Best Child And Preventative Care Clifton Pediatrician Pediatric Care Health

I M Ready For Ivf What Will My Health Insurance Pay For Winfertility



Posting Komentar untuk "Does Bcbs Insurance Cover Ivf"