Covid Testing Covered By Insurance Cigna
This COVID-19 treatment policy applies to customers in the United States who are covered under Cignas employer-union-sponsored insured group health plans insured plans for US-based. Cigna is waiving out-of-pocket costs for FDA-approved COVID-19 diagnostic PCR and antigen testing tests as required by the CARES Act.
According to federal guidelines for insurers health care plans must cover COVID-19 tests when an individual seeks and receives a COVID-19 diagnostic test from a licensed or authorized health care.

Covid testing covered by insurance cigna. In some cases yes. Cigna Health According to its website Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing through Jan. A COVID-19 antibody test looks for antibodies to SARS-CoV-2 the virus that causes COVID-19.
Aetna will waive co-pays for all diagnostic testing related to COVID-19 according to CVS Health. Vaccine guidelines and requirements can vary by state and county. Testing for COVID-19.
All Cigna products and services are provided exclusively by or through operating subsidiaries of Cigna Corporation including Cigna Health and Life Insurance Company Life Insurance Company of North America Cigna Behavioral Health Inc or affiliates and contracted companies. And for its globally mobile customers. Cigna Health and Life Insurance Company Connecticut General Life Insurance Company or their affiliates.
Cigna will reimburse in person visits phone calls real-time synchronous virtual visits and testing for COVID-19 without copay or cost share for all individuals covered under a fully-insured Cigna medical benefit plan and when billed according to the following guidelines. Medicaid patients may not pay out of pocket for Rapid COVID Testing Generally only NAA Test is covered under these health insurance plans Requires telemedicine appointment before scheduling NAA COVID Test BOOK TELEMEDICINE APPOINTMENT. If you test positive for these antibodies it could mean that you already had COVID-19 or that youve been vaccinated for COVID-19.
Generally Rapid COVID-19 testing is not covered but standard PCR testing is usually covered. Self-insured plan sponsors will be. Insurance companies are only required to pay for a COVID.
Eligibility and requirements for COVID testing have expanded since the early months of the pandemic. Cigna Blue Shield Kaiser Are at-home COVID tests covered by insurance. The CARES Act also provides funding to reimburse providers for the cost of administering COVID-19 vaccines to uninsured individuals.
Find vaccine information and resources in your state COVID-19 Vaccines Care and Coverage. This content is offered for informational purposes only. That includes all member costs associated with diagnostic testing for Commercial Medicare and Medicaid lines of business.
Antibodies work to fight illness. The Cigna name logo and ot her Cigna marks are owned by Cigna. Washington Tests to detect antibodies in people who have previously been infected by the coronavirus must be covered free of charge under health insurance plans and Medicaid according to.
BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. In COVID-19 admissions Cigna will allow direct emergent or urgent transfers from an acute inpatient facility to a second acute inpatient facility. HR6201 allows states to use their Medicaid programs to cover COVID-19 testing for uninsured residents and provides federal funding to reimburse providers for COVID-19 testing for uninsured patients.
Cigna Health does not specify a. It does not constitute medical advice. We encourage you and your health care provider to use FDA-authorized tests.
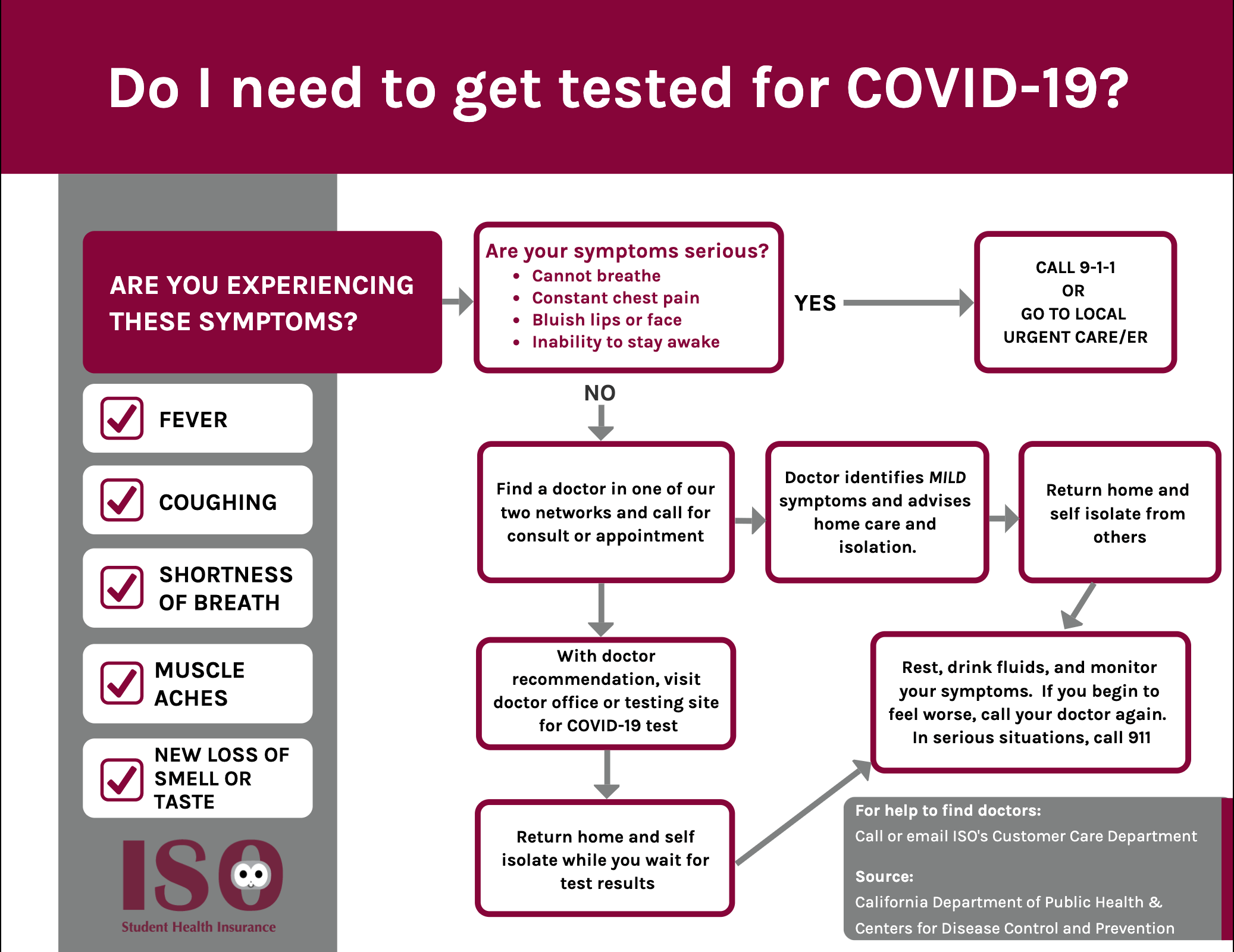
Diagnostic tests determine if you are currently infected with COVID-19. Diagnostic testing generally means a symptomatic or asymptomatic individual seeks and receives a COVID-19 test from a licensed or authorized health care provider or when a licensed or authorized health care provider refers an individual for a COVID-19 diagnostic test ie when an individual customer wants to be tested for any reason and seeks out a test on their own. COVID-19 Tests That Are Supposed To Be Free Can Ring Up Surprising Charges The Families First Coronavirus Response Act passed by Congress requires health plans to fully pay for testing.
There are 2 types of COVID-19 tests. Cigna requires authorization of certain services medications procedures andor equipment prior to. At-home COVID-19 tests must be covered by insurance when the test has been ordered by.
Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers whether at a providers office urgent care center emergency room or via virtual care through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. Cigna Expands and Extends Its COVID-19 Relief Efforts for Medicare Advantage and Individual and Family Plans - Waiving cost share for all in-office or telehealth visits from primary care providers and specialists including behavioral health - Extending previously announced policies including no cost share for COVID-19 testing and treatment. Generally Rapid COVID-19 testing is not covered but standard NAA testing is usually covered.
REQUEST A HOME TESTING KIT This COVID-19 treatment policy applies to customers in the United States who are covered under Cignas employer-union-sponsored insured group health plans insured plans for US-based. Does Cigna Cover Covid testing at urgent care. Coronavirus Resources from the Centers for Disease Control CDC Cigna employs 7000 clinicians including pharmacists medical and behavioral physicians nurses coaches and advisors based on internal HR data as of March 31 2020.
This test can be used to diagnose a past infection with the virus that causes COVID-19. Cigna covers the cost of administering FDA-authorized COVID-19 vaccines at 100 without any out-of-pocket costs when performed by an in-network or out-of-network provider. Testing for COVID-19 is important to slowing the spread of COVID-19.
Medicaid patients may not pay out of pocket for Rapid COVID Testing Generally only PCR Test is covered under these health insurance plans Requires telemedicine appointment before scheduling PCR COVID Test BOOK TELEMEDICINE APPOINTMENT. CI customers will have access to coronavirus COVID-19 testing as prescribed by health practitioners and the company will waive all co-pays or cost-shares to help fight the rapid spread of the virus in the US.

Manipal Cigna Health Insurance Plans Reviews And Premium Calculator
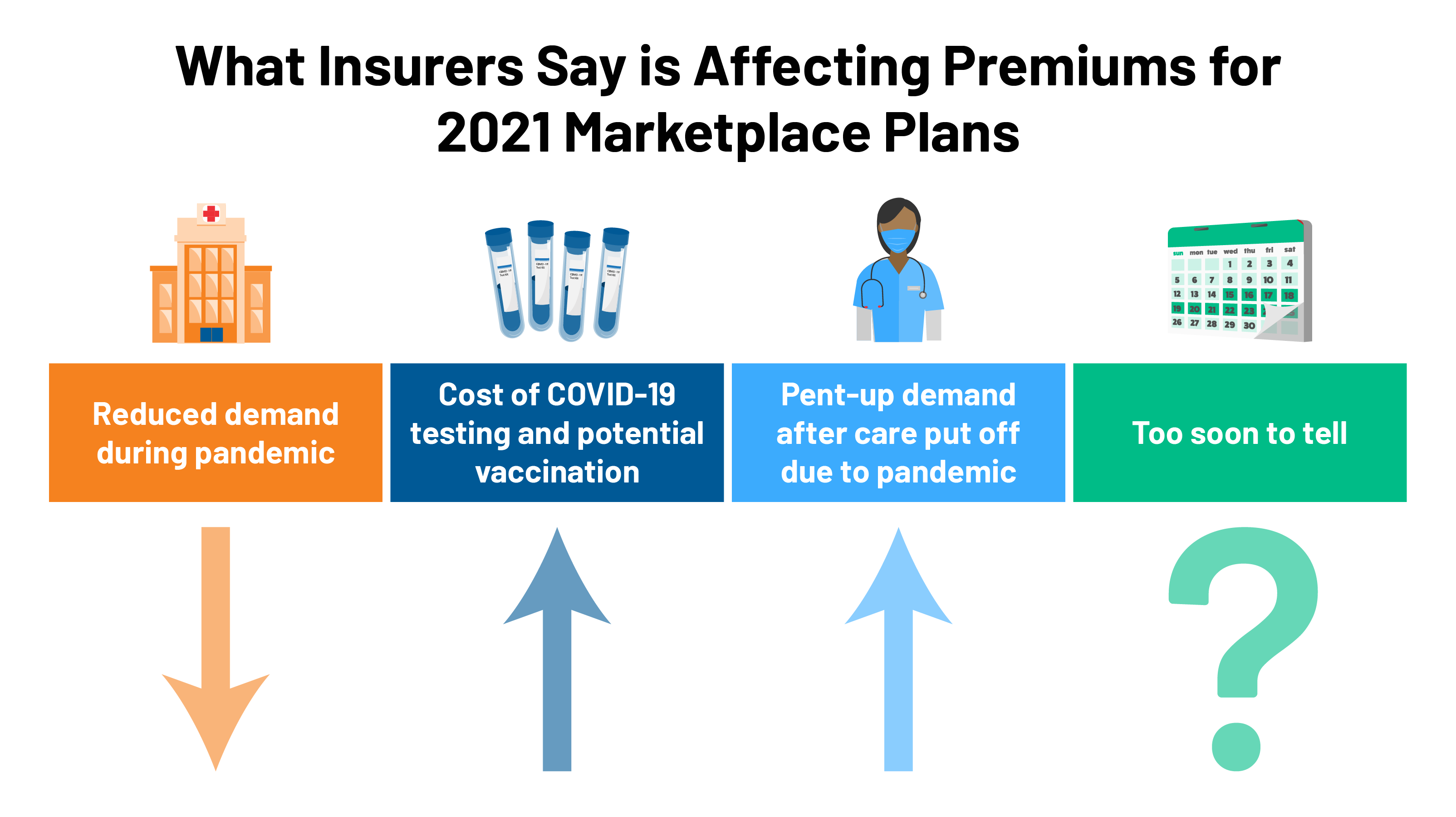
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Cigna And Humana Waive Coronavirus Treatment Costs

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Cigna Protects Its Workforce By Requiring Covid 19 Vaccinations Or Testing For Employees Entering U S Worksites

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Health Insurer Cigna To Expand Obamacare To Three New U S States Reuters

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Cigna Raises Financial Forecast For 2021 Despite The Ongoing Covid 19 Pandemic Healthcare Finance News
Iso International Student Insurance

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Covid 19 Pruebas Tratamiento Y Cobertura De La Vacuna Cigna

What To Know About Coronavirus Your Insurance Utah Insurance Department

Posting Komentar untuk "Covid Testing Covered By Insurance Cigna"