Does Insurance Cover Covid Testing For Travel Aetna
Taking COVID-19 testing on the road. Aetna does not specify a limit on the number of COVID-19 tests which it will cover.

Cvs Profits Rise As Patients Postpone Care Aetna Pays For In Pandemic
A spokesperson from the Insurance Council of Australia told Canstar that travel insurance would be available with some COVID-19-related cover to any countries who may have their Do Not Travel warnings lifted in the coming months by the Australian Government.

Does insurance cover covid testing for travel aetna. Worksite Labs conducts tests in Ft. COVID-19 vaccines and diagnostic testing continue to be covered 100 percent by Aetna in line with. We do not cover the cost of antibody testing.
We only cover the cost of PCR testing when requested by a medical professional. Patients can book an appointment online visit the mobile clinic without waiting in line get tested and learn. This policy covers the cost of the office clinic or emergency room visit that results in the administration of or order for a COVID-19 test.
Our diagnostic test is quick easy and effective. Anthem also confirms that prior authorization is not required for diagnostic services related to COVID-19 testing. Carbon Health in partnership with Studio Dental is taking its mobile COVID-19 testing clinic to stops throughout the Bay Area and beyond.
Does my health insurance cover testing and treatment for COVID-19. Testing is free with insurance plus a 35 charge for next-day results or 75 for same-day results. In fact Aetna says deductible-free inpatient treatment for COVID-19 expired in late February.
If you are worried that you may have been exposed to COVID-19 please contact us. The test can be done by any approved. First youre doing the smart thing by getting tested before traveling.
Airlines and travel providers may also enforce COVID-19 testing for travellers prior to departure. The Families First Coronavirus Response Act and CARES Act do not require an insurance company to pay for a test unless you have symptoms or a known or recent exposure to COVID-19 and it has been determined to be medically necessary for you by an attending healthcare provider. 1-800-557-6059 TTY 711 247.
Aetna is not limiting the number of diagnostic testing we will cover for members however all tests must still meet the requirements listed in this section for coverage. Anthem Blue Cross Blue Shield. Lauderdale West Palm Beach and Miami.
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a doctor. Will Aetna cover other virus testing if those services are for the purposes of COVID-19 testing. Aetna will waive co-pays for all SARS-CoV-2 testing for all insured enrollees whether the enrollees are in commercial Medicare or Medicaid plans.
The cost is 90 for results in 24 hours or 150 for results in 12 hours. The following insurers and their responses to COVID-19 can be found below and will be updated when new information is provided by insurers. As stated above we only cover COVID-19 diagnostic testing when a member has been referred by a licensed physician.
And second youre in luck. Anthem will cover the cost of coronavirus testing with no out-of-pocket cost. Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you.
One of the most pressing questions. For further details on testing and our policy please refer to Will you pay for the cost of COVID 19 testing below. The following rates are used for COVID-19 testing for commercial and Medicare plans unless noted otherwise.
The company recommends using telehealth when possible to help prevent the spread of a virus. Covid Testing LLC does testing at several locations in Orlando and Central Florida. Some countries require COVID-19 testing for travellers on arrival.
Effective immediately Aetna members will have access to the following resources. We dont cover mandatory testing for travellers either on arrival or departure well only provide cover for. And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19 test will only be a covered cost under.
Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently. To ensure access for COVID-19 testing and have consistent reimbursement Aetna will reimburse contracted and non-contracted providers for COVID-19 testing as follows in accordance with the members benefit plan 3. Will mandatory testing be covered.
Some countries require COVID-19 testing for travelers. As of 6192020 Routine testing for influenza strep and other respiratory infections without a COVID-19 test will be covered subject to applicable cost sharing under the members plan. Our Health Care Hacker Jonathon Hess of Athos Health has some tips for finding the answers.
Carriers in Nebraska regarding the Coronavirus also known as COVID-19. And we dont cover COVID-19 antibody testing. This is because insurance companies will consider COVID-19 as a pre-existing condition.
Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings. If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. Aetna will waive member cost sharing for diagnostic testing related to COVID-19.
Yes most likely you can still get health insurance if you have been diagnosed with COVID-19 but the insurance company might exclude Coronavirus from your coverage. Under the Act public and private insurance including self-funded plans have to cover FDA-approved coronavirus tests and costs associated with diagnostic testing. But the federal Families First Coronavirus Response Act does not require insurers to pay for tests to monitor workplace safety or for public health surveillance said Kristine Grow a spokeswoman.
Health Care Plan Benefits Human Resources Vanderbilt University
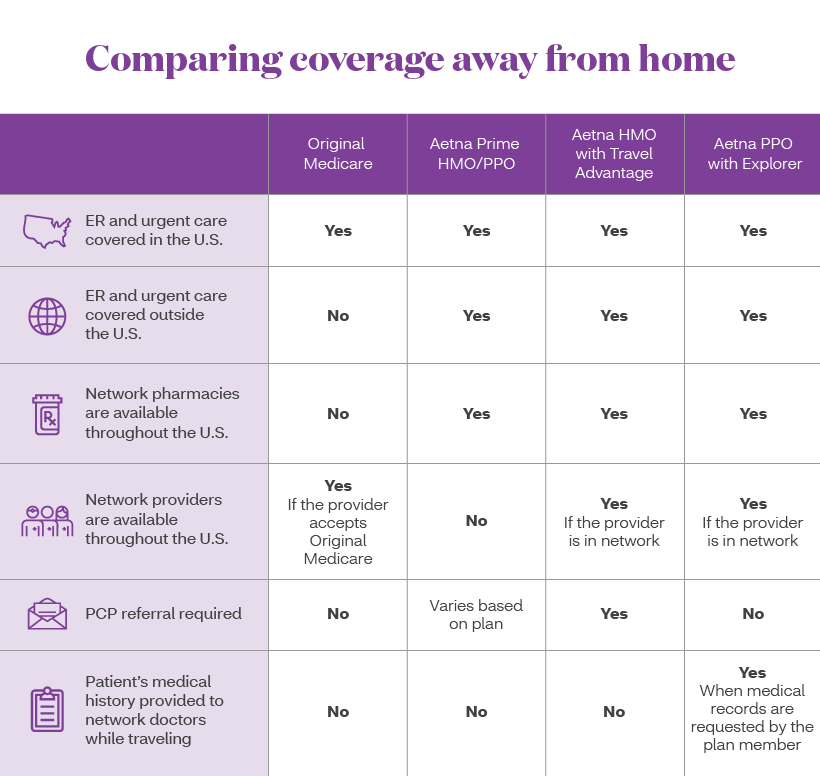
The Right Medicare Coverage For Travelers Aetna
Coronavirus Covid 19 Taking Action Aetna

Telehealth And Covid 19 Billing And Coding Resources
Insurance Carecube We Take Most Of Major Insurances
Epo Health Insurance Plans From Aetna Exclusive Provider Organization Health Care Coverage

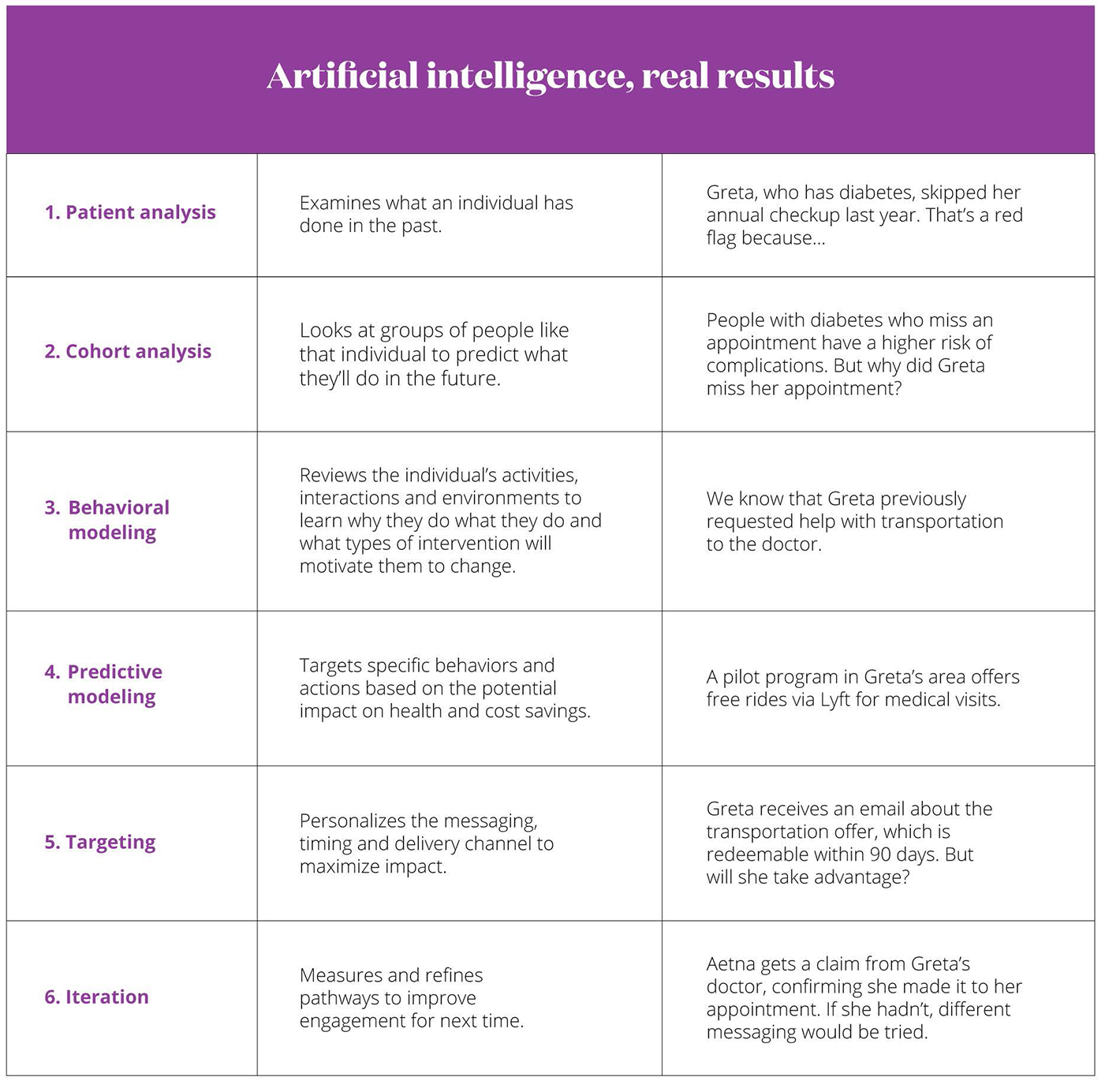
Personalized Customer Service Programs Support Aetna

Does Your Health Insurance Cover You For Covid 19 Cbs News

Epo Health Insurance Plans From Aetna Exclusive Provider Organization Health Care Coverage

Covid Testing Care Station Medical Group

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

What To Know About Coronavirus Your Insurance Utah Insurance Department

Mental Health Insurance Plans Coverage From Aetna Behavioral Health Benefits Programs For Employers

Aetna Insurance Exaggerated About Pediatricians In Its Network Federal Whistleblower Suit Claims Pittsburgh Post Gazette

Tips To Make Getting Healthy Easier Aetna

Un New York Health Insurance Plans United Nations

Aetna Health Life Insurance Section


Posting Komentar untuk "Does Insurance Cover Covid Testing For Travel Aetna"