Does Insurance Cover Urgent Care Covid Testing
They offer primary care services and the wait time can be much shorter than an ER visit. The federal government requires insurers to cover diagnostic Covid-19 testing and the related visit without a copay a policy that includes patients who.
Any medically necessary treatment for COVID-19 is covered under MITs StudentAffiliate Extended Insurance Plans.

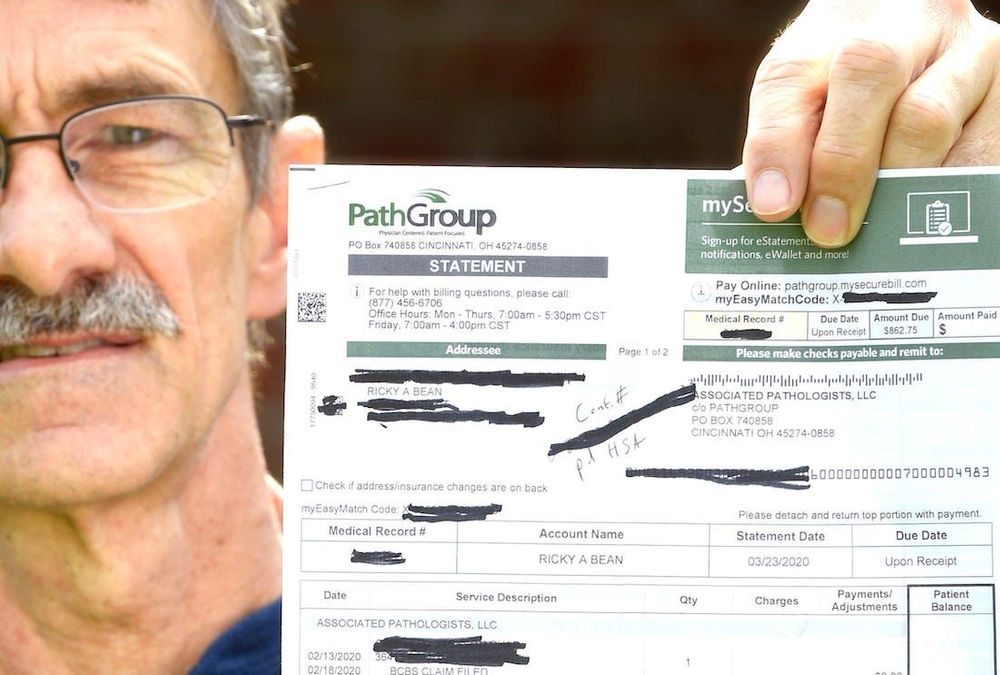
Does insurance cover urgent care covid testing. Blue Cross Blue Shield will cover the full cost of diagnostic tests for COVID-19 for individuals who meet the Centers for Disease Control and Prevention CDC guidelines for testing provided that the test meets CDC guidelines. PEBTFRetired Employees Health Program REHP medical plans will waive all deductibles coinsurance and copays for diagnostic testing and in-network inpatient hospital care emergency room or urgent care for COVID-19. Can I pay out of pocket.
However not every insurance company covers the cost of rapid tests in which the patient would be responsible for the cost of that test. MedicareMedicaid Patients - The cost. Please check your Evidence of Coverage or plan policy documents to find out what is.
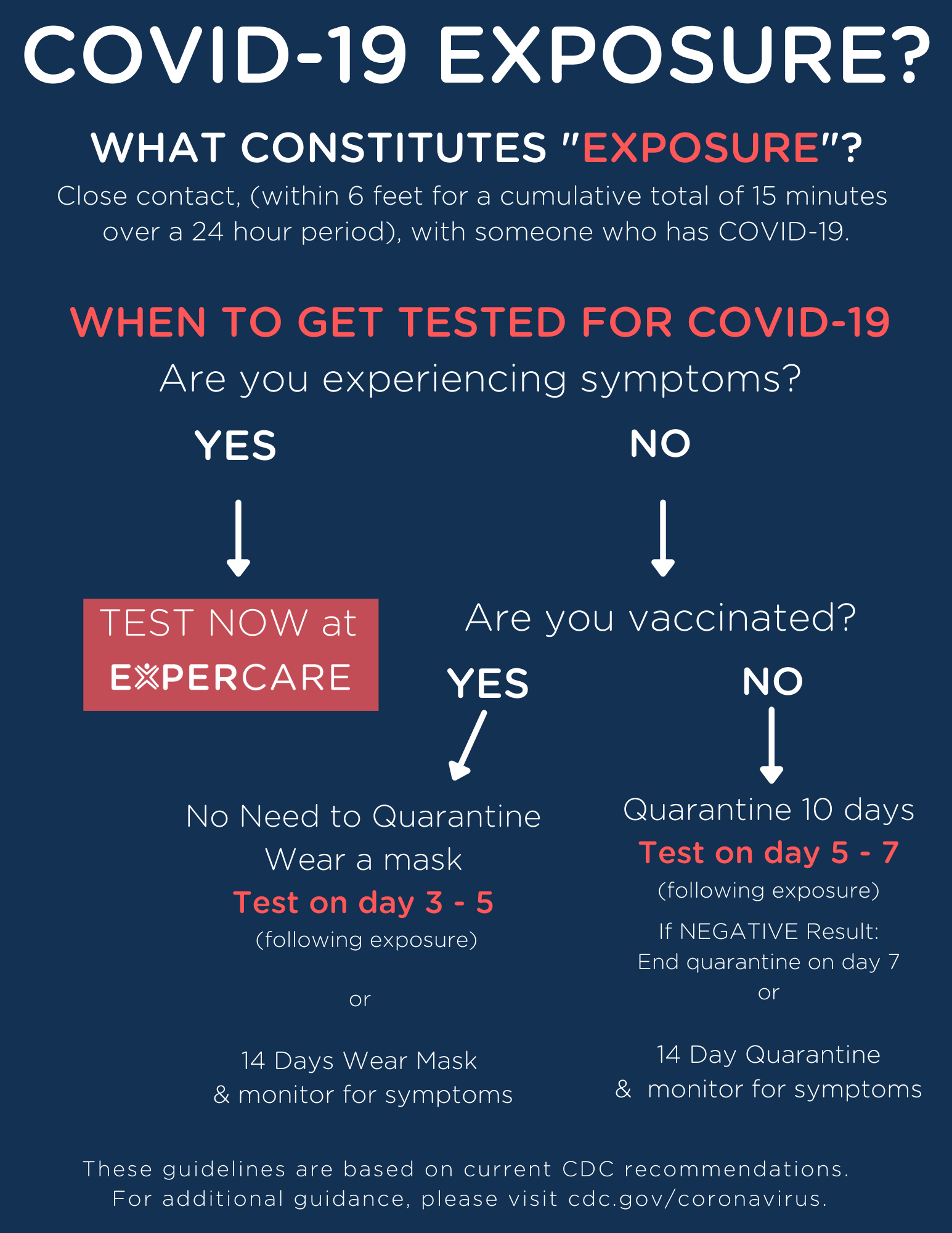
Drivers License Passport etc Q. Are experiencing and COVID-19 symptoms such as fever cough shortness of breath sore throat or generally feeling weak. However if you fall ill with COVID-19 like symptoms while traveling testing and treatment may be covered if appropriate documentation is submitted.
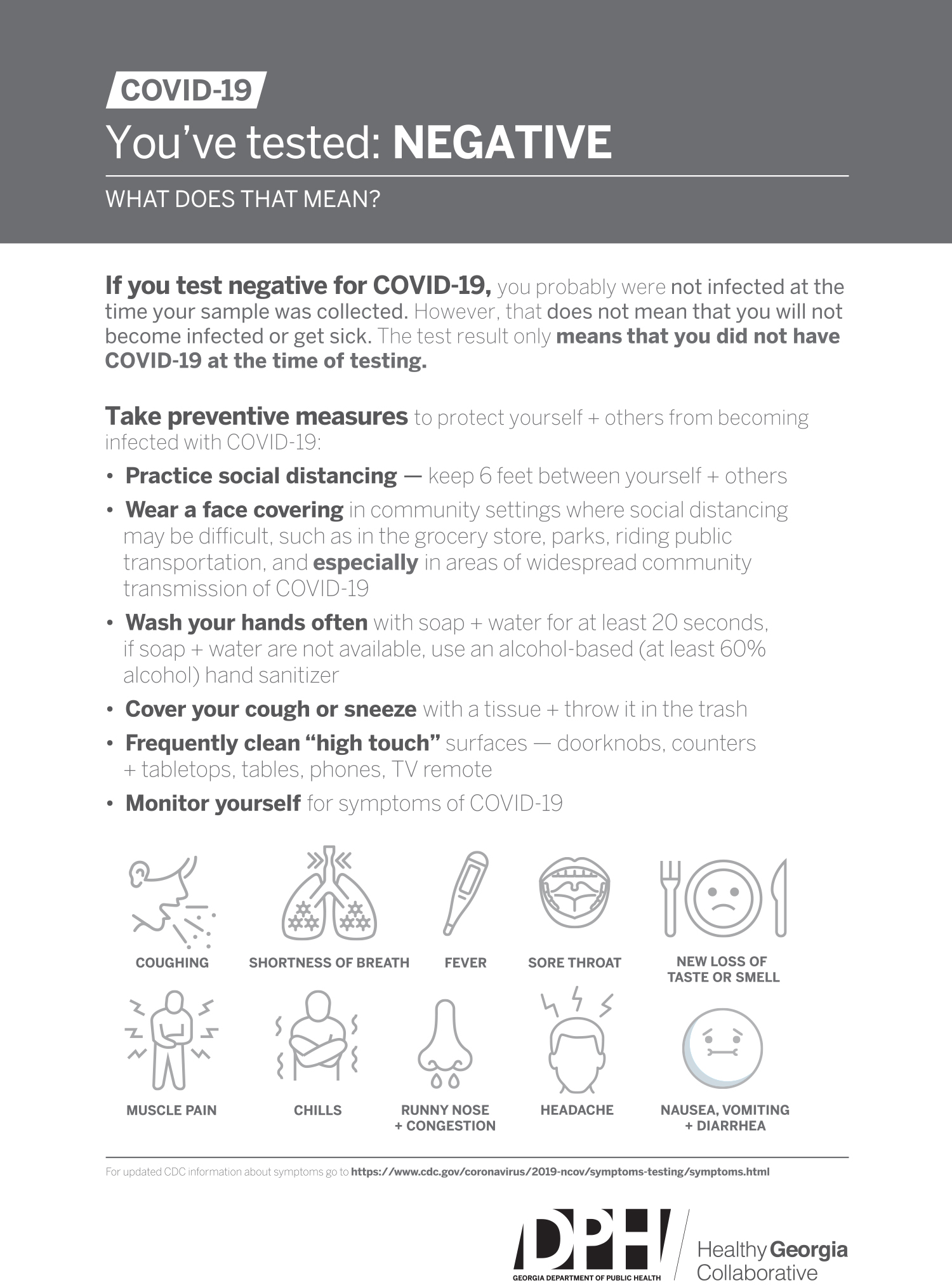
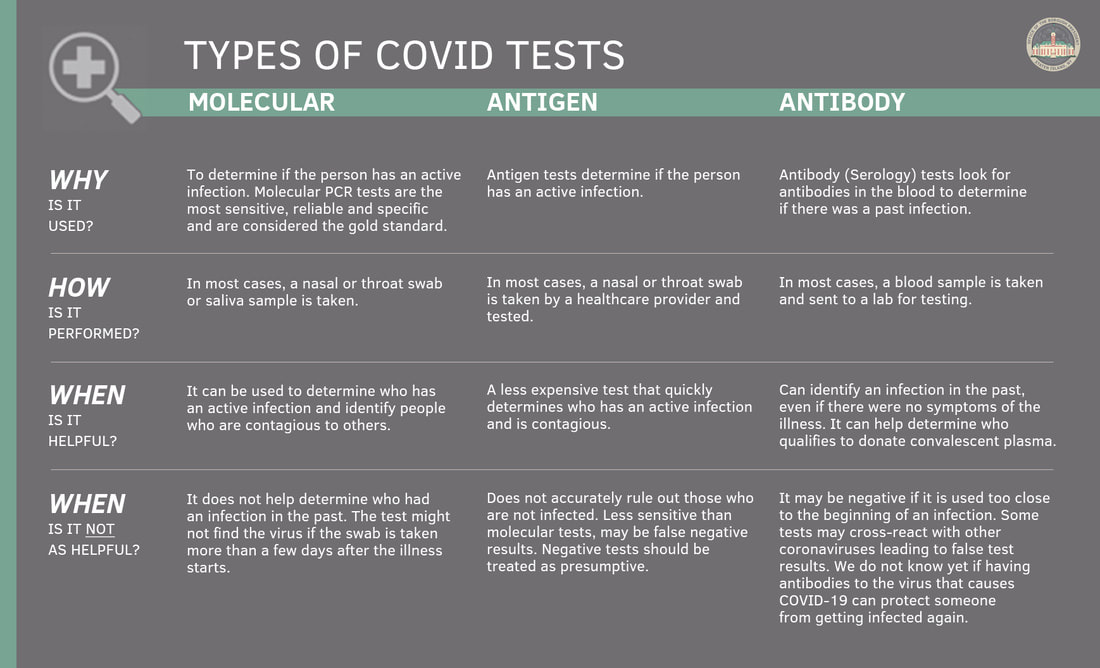
And they can let you know if you need emergency care. Antibody tests are used to test for antibodies to the coronavirus COVID-19 in your blood. BCBSIL is waiving your share of the costs for COVID-19 testing and testing-related visits until the end of the Health and Human Services COVID-19 public health emergency order.
The policy will cover the test kit for members who meet Centers for Disease Control and Prevention. Eligible Veterans will not be charged a copayment for COVID-19 viral testing. State variations and regulations may apply.
UnityPoint Health is encouraging people to get tested at the onset of COVID-19 symptoms. We offer testing to determine whether you are currently infected with COVID-19 through diagnostic molecular testing or an Active Infection Test. What if I do not have insurance.
For some plans only emergency and urgent care are covered internationally and COVID-19 testing for routine travel does not qualify as urgent or emergency care. Please call your local CareNow urgent care if you have any questions. Most health insurance plans do not cover COVID-19 tests for reasons other than diagnosis or treatment by a health care professional.
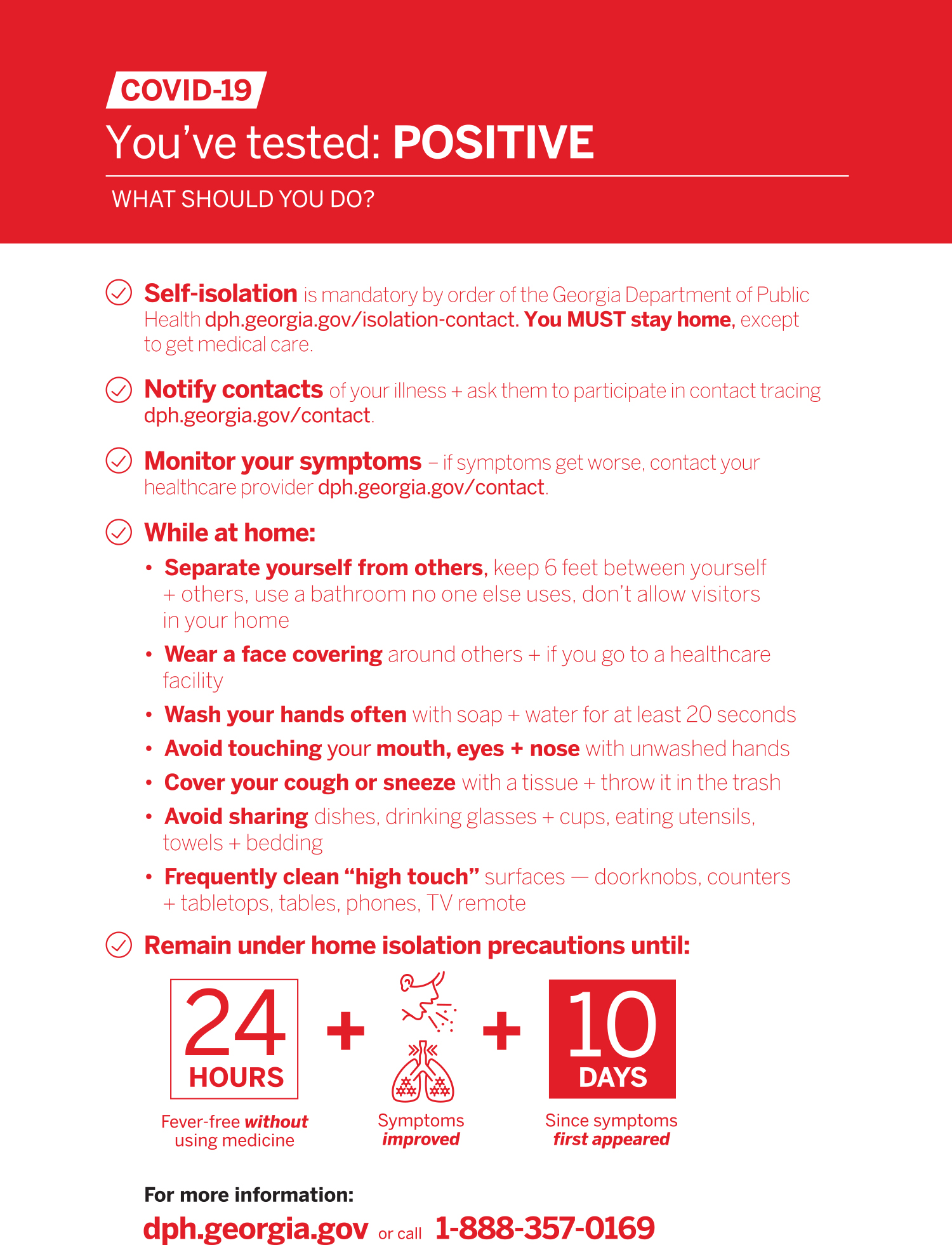
Yes in most cases. Monoclonal antibody treatment is effective in keeping COVID-19 positive patients out of the hospital but it needs to be administered early on in the disease. You will be asked to provide your social security number and a government issued ID ie.
We anticipate your test results will be available within 48 hours. UnitedHealthcare will cover medically appropriate COVID-19 testing at no cost share during the national public health emergency period currently scheduled to end Oct. What are private health insurance plans required to cover.
If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. This page helps uninsured individuals find no-cost COVID-19 testing treatment and vaccines. UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment.
A swab test is appropriate if you. CareNow urgent care can provide COVID-19 testing for those who are experiencing coronavirus-like symptoms. This is to see if you previously had been infected with COVID-19.
AFC Urgent Care participates in a federal program to cover the cost of testing. In-network Urgent CareRetail locations if it is in conjunction with a clinical visit for care. These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan.
The Department of Insurance issued a Bulletin IC-39 strongly encouraging carriers to waive costs so you will not have to pay your copayment coinsurance or deductible when you go to your in-network doctor an in-network provider at another outpatient setting an in-network urgent care center or an emergency room to diagnose COVID-19 including when the services are provided through telehealth. Medicare does cover urgent care visits. Health plans cannot decline to cover office telehealth urgent care or emergency room visit that results in an order for a COVID-19 test and cannot charge any cost-sharing from the patient.
Most private group and individual market plans including grandfathered plans which are plans that existed before the 2010 Affordable Care Act and have not changed significantly since must cover COVID-19 testing and diagnosis without charging enrollees cost sharing such as copayments or deductibles. If you do not have health insurance talk to any health care provider in your area to see if they will agree to bill the federal government for other COVID-19 related care like testing and. You must truly be uninsured or not be covered under another policy to qualify.
VA will reimburse community providers for COVID-19 viral testing of eligible Veterans at one of the following outlets. Most insurance companies cover the cost of COVID testing with no out-of-pocket expense. COVID-19 vaccines are 100 free for every individual living in the United States - even if you do not have insurance.
If you have parts A and B known as original Medicare Part B will cover your urgent care. Your plan will cover diagnosis testing and treatment associated with COVID-19 including. Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers whether at a providers office urgent care center emergency room or via virtual care through the Public Health Emergency PHE period currently scheduled to end on October 18 2021.
Have been exposed to COVID-19 in the last 14 days. Burbank Urgent Care offers Rapid Antigen Testing with same day results as well as Antibody Blood Testing to view if you have antibodies in relation to the coronavirus from a past infection. For example tests conducted for return to work purposes or travel are generally not covered.
Testing earlier means more treatment options may be available for you. Since the legislation was passed on March 18 2020 all forms of public and private insurance are required to cover the costs of COVID-19 testing. The cost to you will depend on the Medicare plan that you have.
17 2021 when ordered by a physician or appropriately licensed health care professional for purposes of the diagnosis or treatment of an individual member. If you have coverage through the Pennsylvania Employee Benefit Trust Fund PEBTF.
How Much Does A Rapid Covid 19 Test Cost Without Insurance Mira

Drive Through Covid Testing Lafayette Concord Pleasant Hill Livermore Click To Register To Schedule

Covid 19 Testing For Kids Children S Healthcare Of Atlanta
Private Health Coverage Of Covid 19 Key Facts And Issues Kff

Covid 19 Testing Nj Am Pm Walk In Urgent Care Coronavirus Testing

Covid 19 Testing Healthcare Services In New York Multi Specialty Practices

Covid 19 Testing Gohealth Urgent Care

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
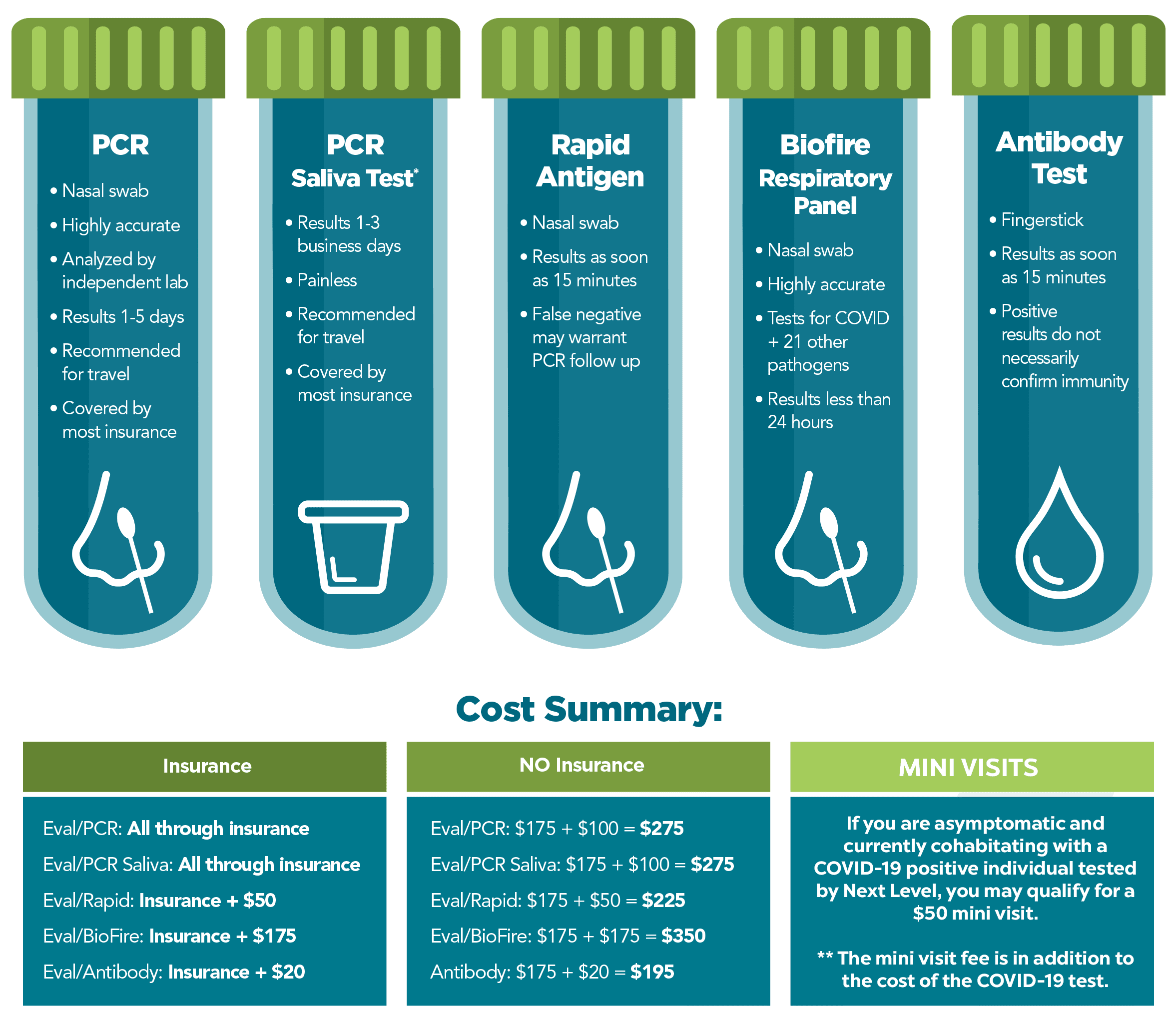
Covid 19 Testing Next Level Urgent Care

Excel Urgent Care Of Iselin Nj Walk In Urgent Care Located In Iselin Nj

How Much Does The Urgent Care Cost

Drive Thru Covid 19 Testing In Livermore California Urgent Care In Clinic And Video Visits Stat Med Urgent Care

San Marcos Urgent Care Covid19 Testing Center Is Available Open 7 Days
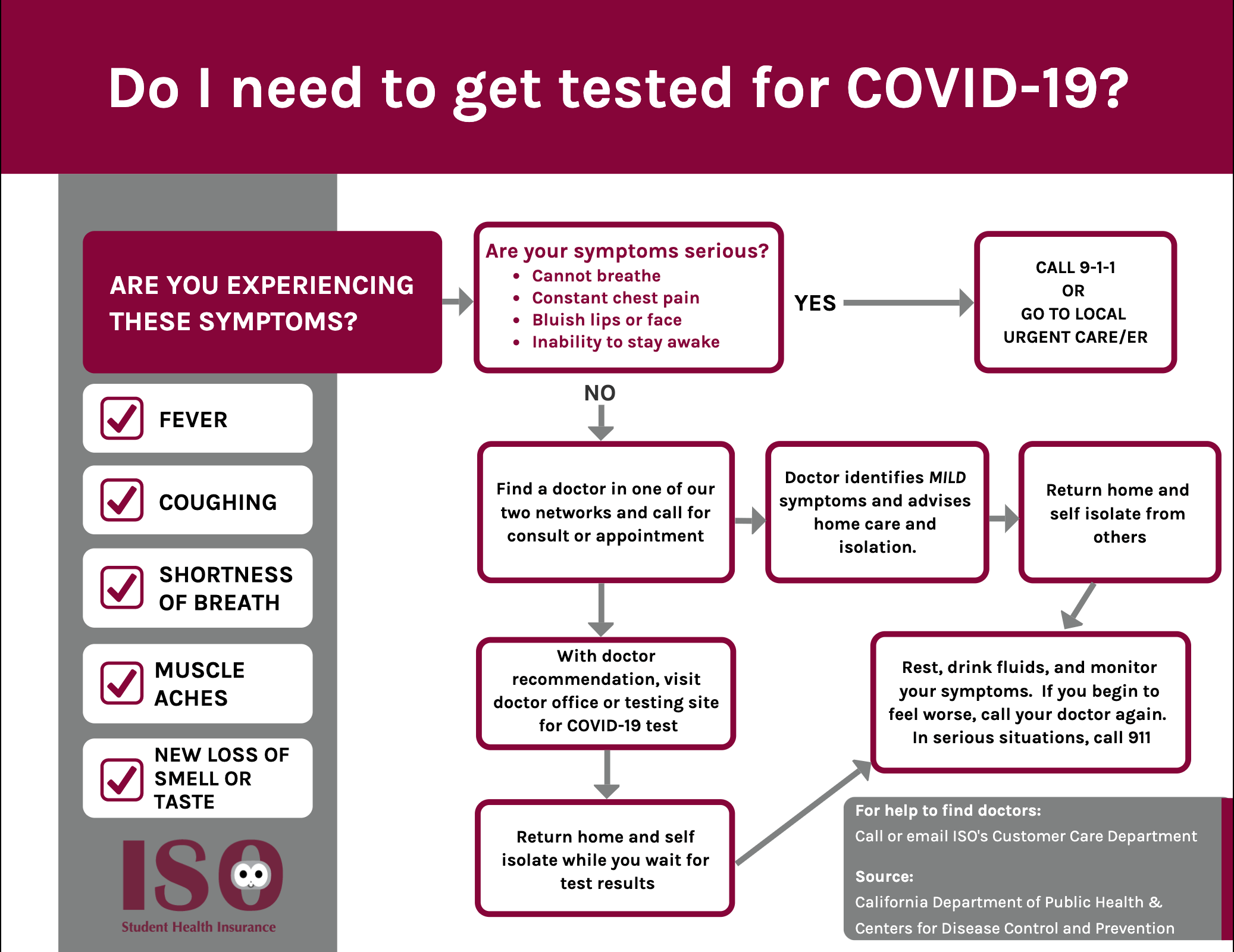
Iso International Student Insurance


Posting Komentar untuk "Does Insurance Cover Urgent Care Covid Testing"